Breasts may become droopy with age or following pregnancy or significant loss of weight. Both physical and psychological health can be affected in women with empty droopy breasts. One can get rashes and infections underneath the breasts. Patient have to wear a padded bra to maintain shape and volume of their breasts. Patients are not keen on exposing themselves in front of their partners and have poor body image.
An augmentation mastopexy procedure helps restore volume and shape to the breasts. Some surgeons are not comfortable with performing the two procedures as a single procedure. Having trained in Stockholm with Dr Per Heden who has mastered the art of doing the procedure as a single stage and has taught surgeons around the world about it, Mr Mahajan is happy to offer a single stage procedure to his patients.
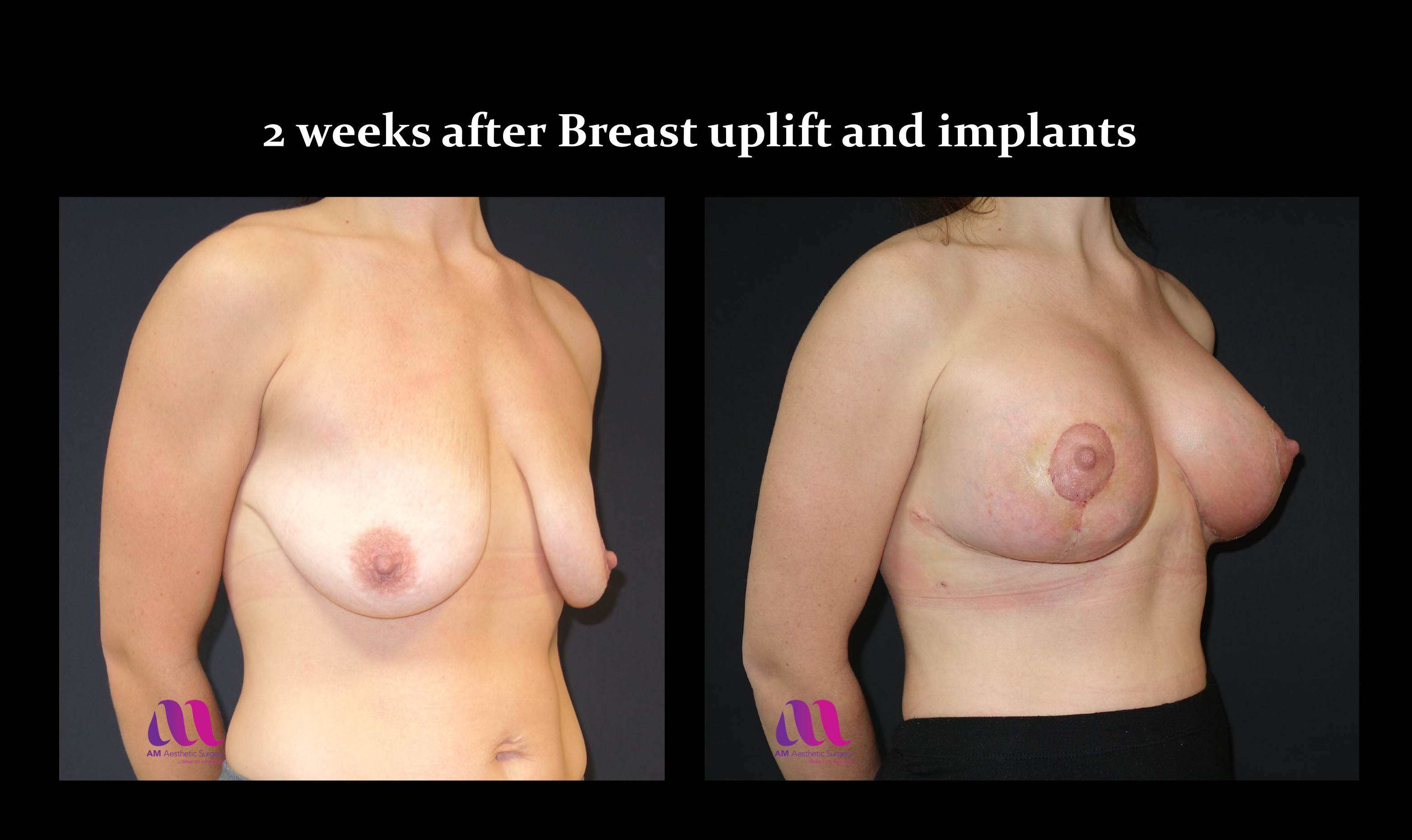
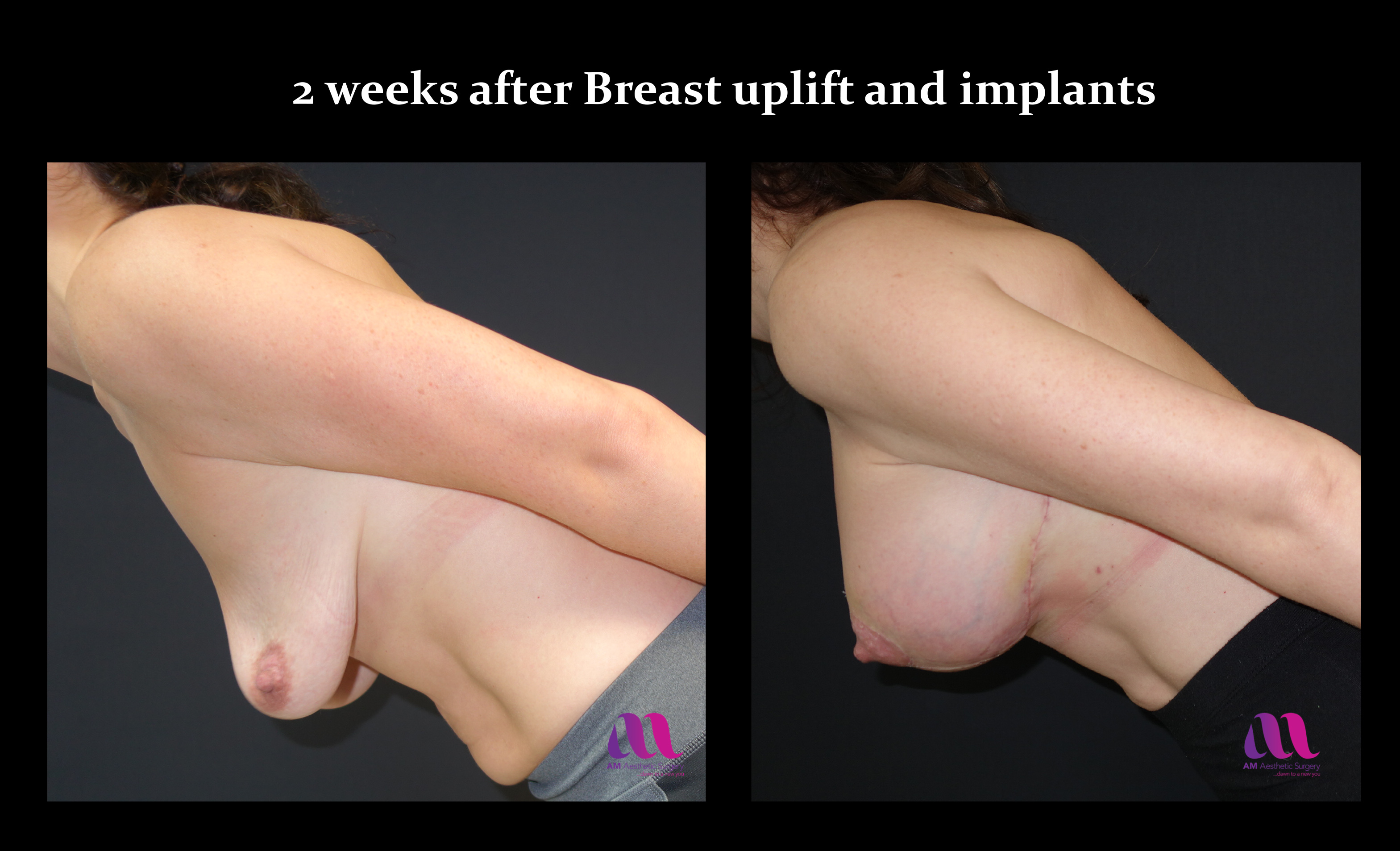
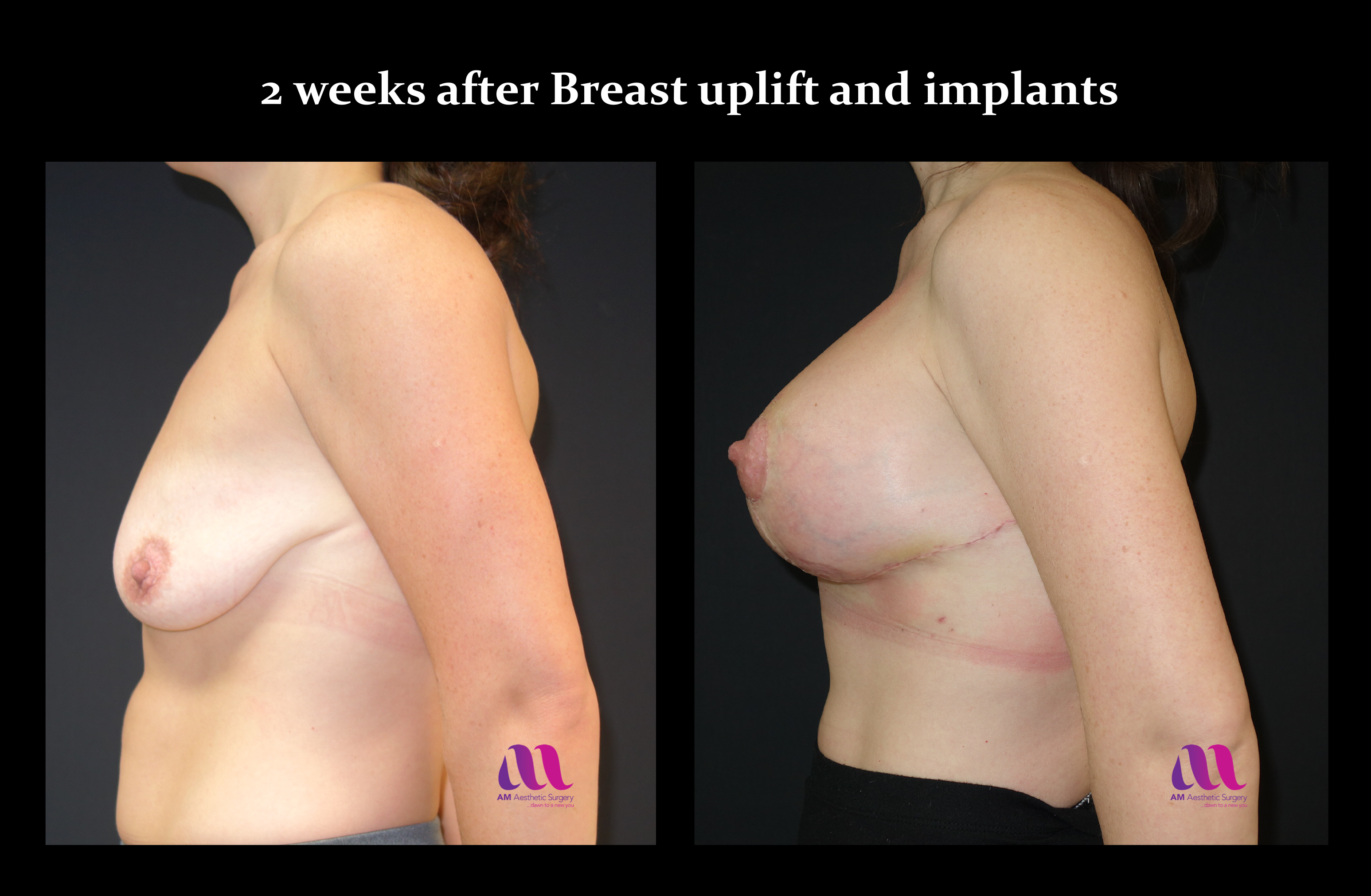
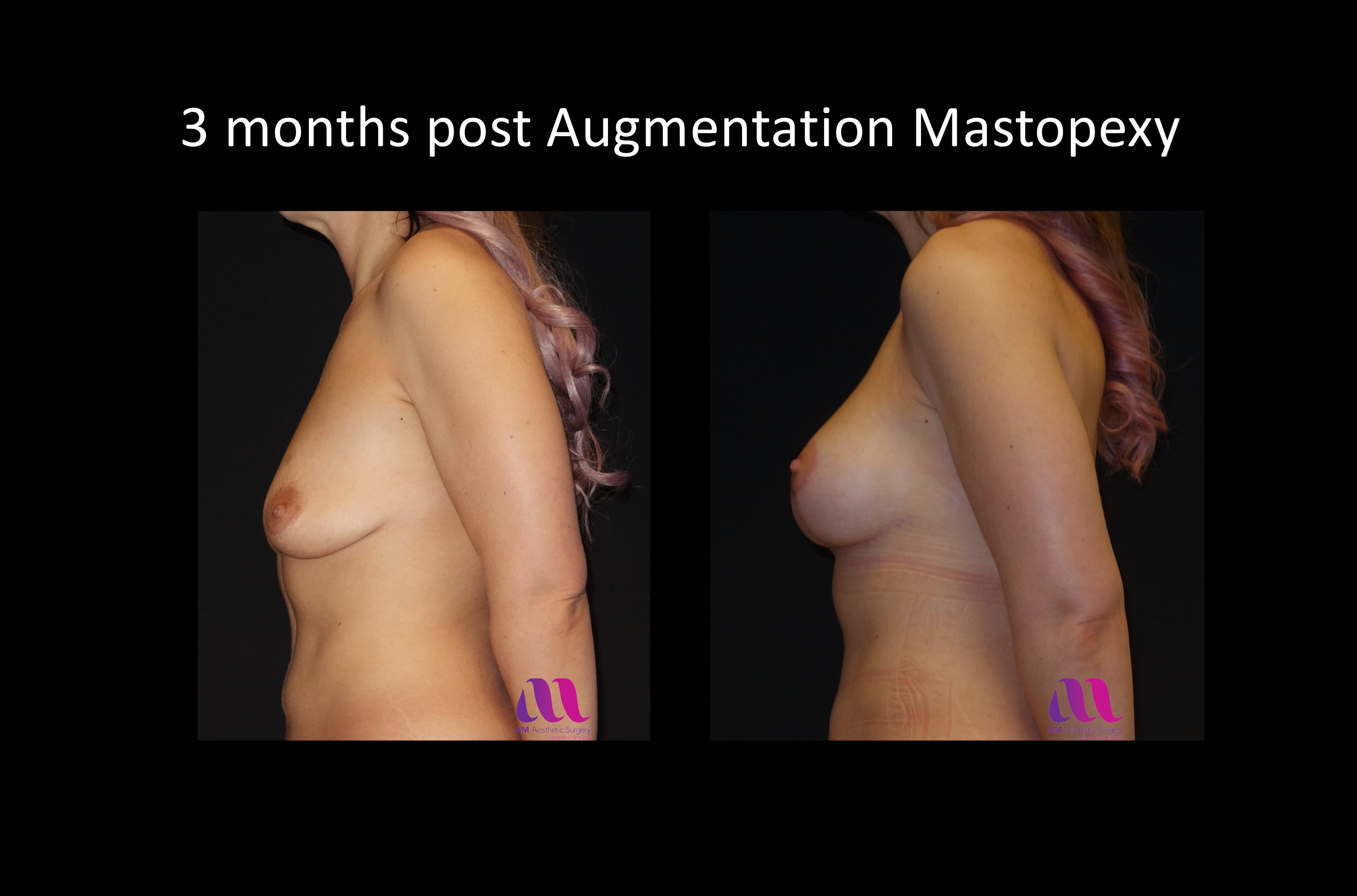
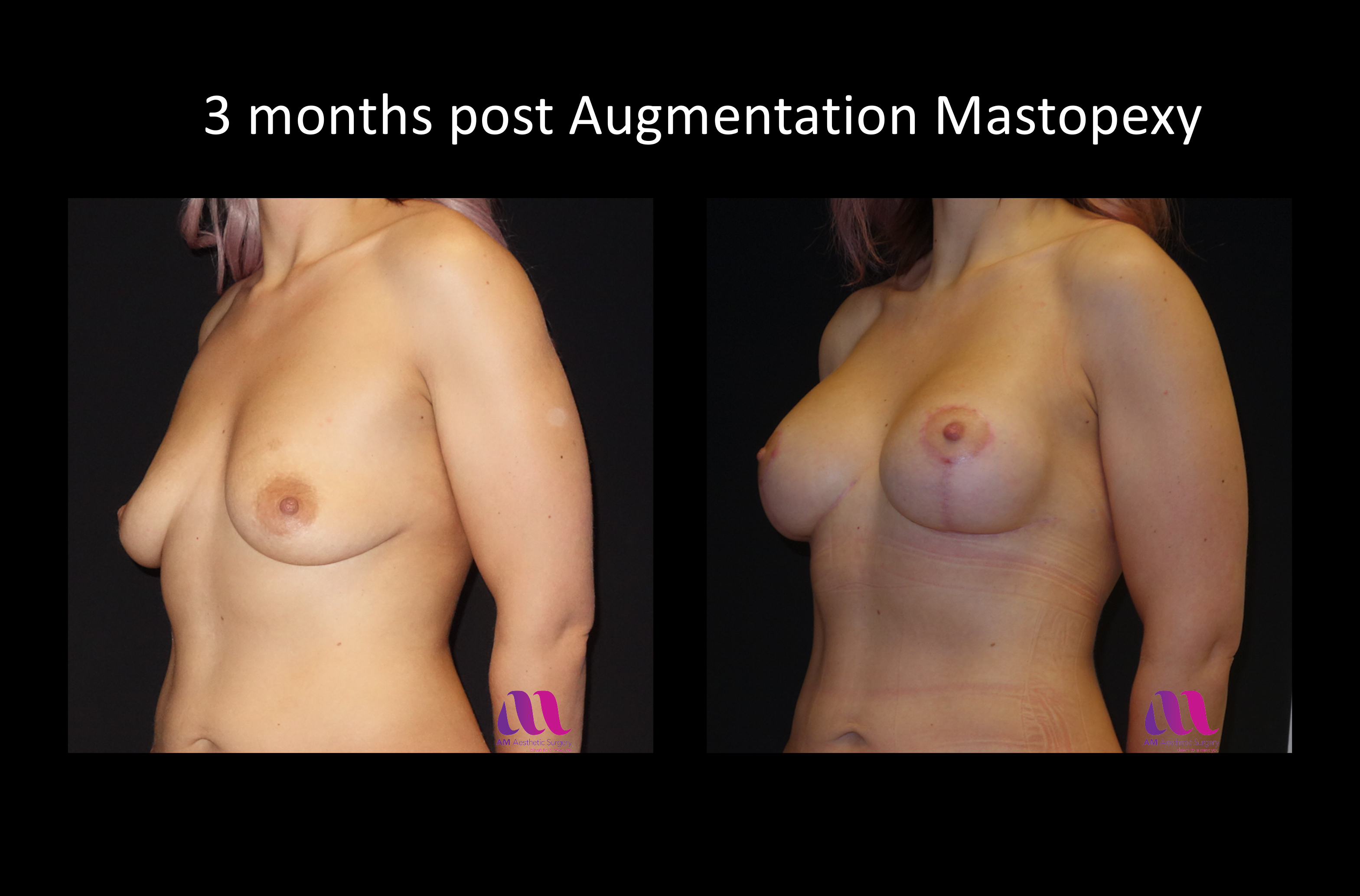
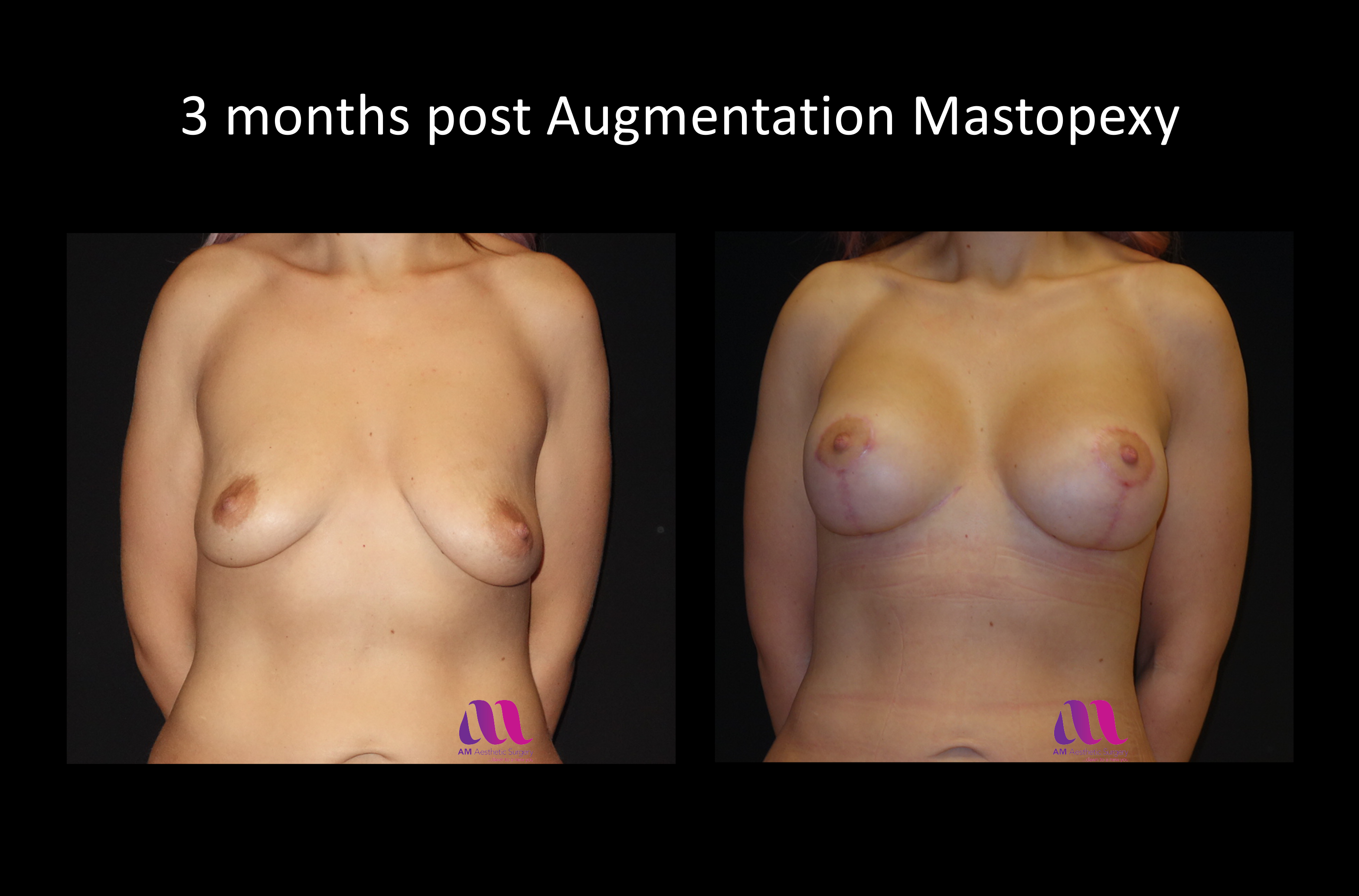
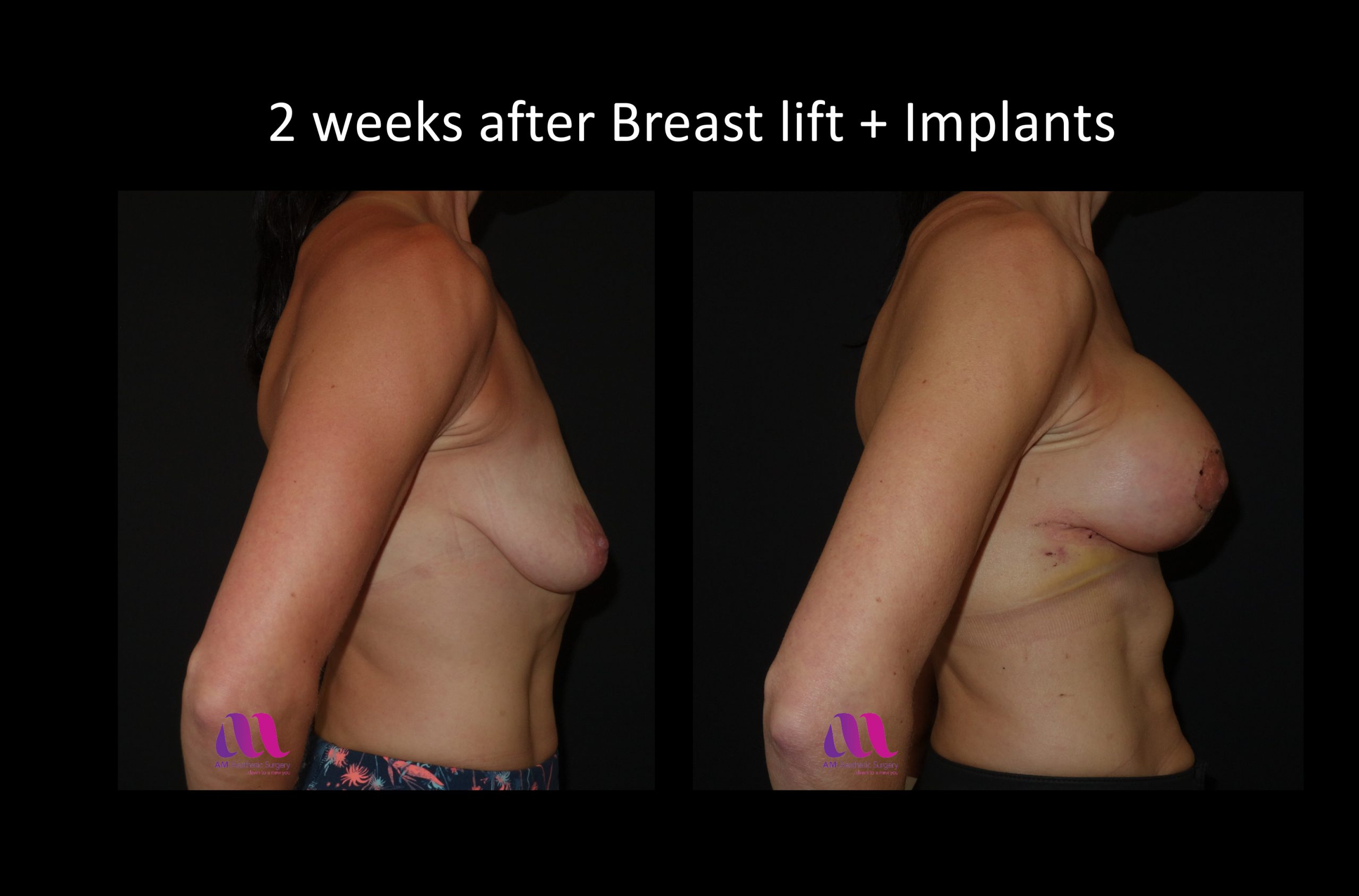
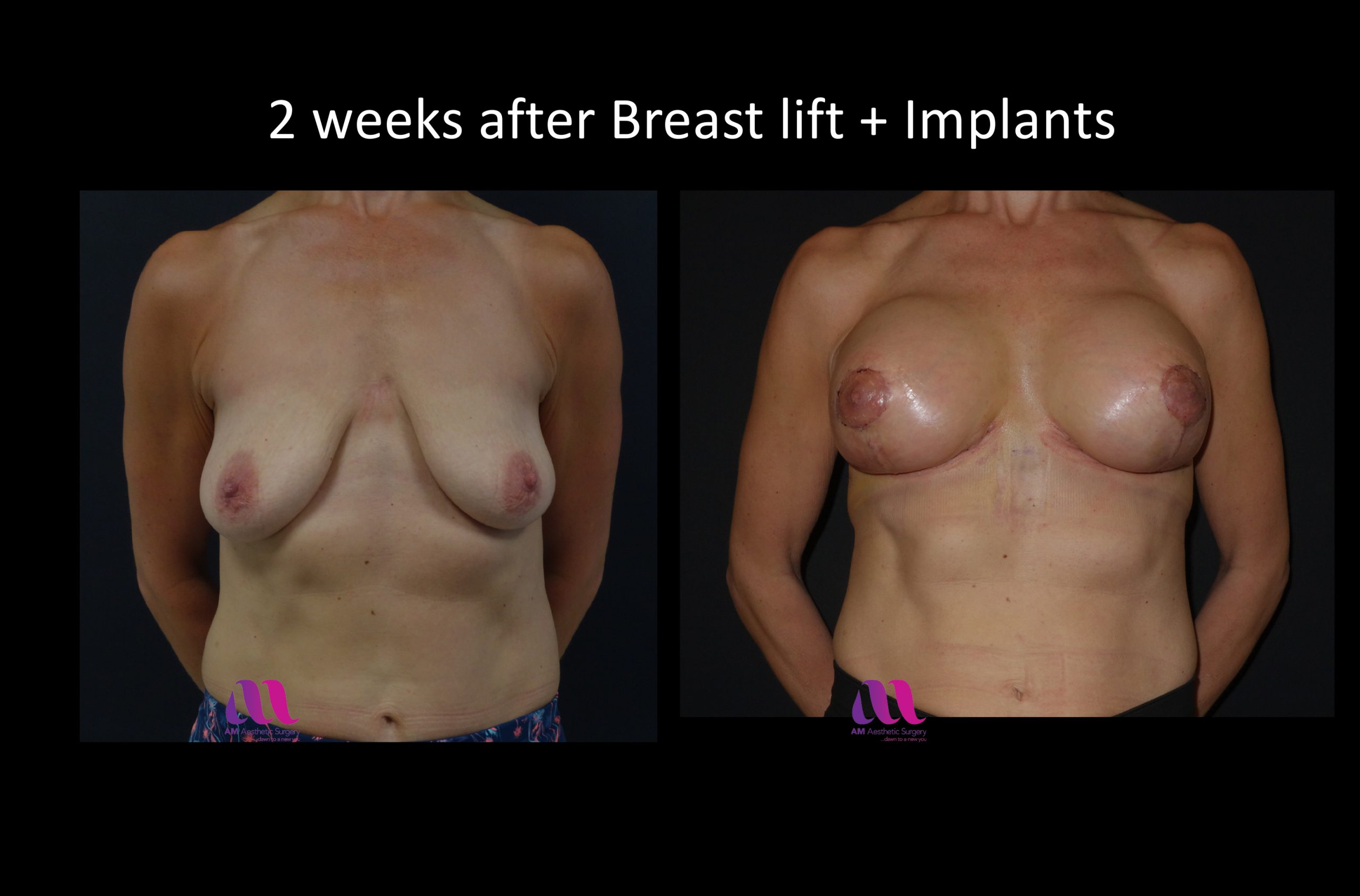
An augmentation mastopexy procedure enhances the volume of your breasts and tailor tacks your breast envelope to fit the new breast volume. Following the procedure, patients have a nice shape to their breasts and the nipples are elevated and placed in the right position on the newly enhanced breasts. In the end, the breasts are no longer saggy and are much more fuller, perkier and attractive. Some patients have a very large areola which can be reduced to a smaller, regular and well defined areola that is much more desirable.
Patients often come to us for this procedure after contemplating about it for years. After the procedure, they wish that they had had it done ages ago and not had to live with their empty saggy breasts for all those years.
WHO IS BREAST AUGMENTATION MASTOPEXY FOR?
- Breast that are empty and stretched down with loss of shape – Droopy and saggy.
- Breasts with large areola
- If you are not happy with volume of your breasts in a bra and their shape
- Associated symptoms of rash or infections under breasts
BENEFITS OF BREAST AUGMENTATION MASTOPEXY
- Enhances volume of your breasts
- Uplifts breasts and makes them perkier
- Reduction of associated symptoms of rash or infections
- Smaller and aesthetically pleasing areola
BREAST AUGMENTATION MASTOPEXY METHODS
- Wise pattern or Key hole or inverted ‘T’ pattern reduction
- Vertical short or ‘lolipop’ scar reduction
- Peri areolar or ‘doughnut’ scar
- Minimal scar breast uplift
CHOICE OF BREAST IMPLANTS
- Saline filled breast Implant
- Silicone gel breast Implant
- Anatomical shaped or ‘tear drop’ breast Implants
- Round shaped breast Implants
BREAST IMPLANT PLACEMENT
- Subglandular position under the breast gland and above the muscle
- Submuscular position under the muscle
- Dual Plane technique involving positioning the implant partially under the muscle and partially under the gland / subcutaneous tissue
BREAST AUGMENTATION MASTOPEXY NEED-TO-KNOW INFO
- Duration of surgery: 3 to 4 hours
- Anaesthesia: General Anaesthetic
- Duration of inpatient stay: 1 to 2 days
- Wounds healed in: 2 weeks
- Scars matured in: Settle in 3 to 6 months, Fully matured in 12 to 18 months
- Back to light work: 1-2 weeks
- Back to cardiac exercise / fast walking: 2 weeks
- Back to labour intensive work / Exercise: 4 to 6 weeks
- Sexual activity: 4 to 6 weeks
- Able to drive: 2 weeks (Should be able to apply emergency stop)
- ‘Long haul’ flights / holidays: Avoid four weeks before and after. Short flights are okay.
- Shower / bath: Keep dressings dry for 2 weeks
- Sun bathe: Keep the scars covered or protected with a high factor sun protection cream until they mature in about a year or so.
- Garments: Sports bra for 8 to 12 weeks
- Post operative review: 2 weeks, 3 months (As often as necessary if clinically indicated)
- Post Operative pain / discomfort: 2 to 7 days
- Potential risks: (Every effort is made to reduce the risk of complications, but potential risks are) Bleeding, bruising, swelling, haematoma / seroma, infection, explantation of the implant, delayed wound healing, scars – hypertrophic, stretched, sensitive, not in the inframammary crease, no guarantee of cup size or cleavage, altered sensation – decreased or increased, altered lactation and mammogram, asymmetry, nipple loss, fat necrosis, Implant – visibility, palpability, rippling, rotation, rupture, silicone granuloma / axillary lymphadenopathy, capsular contracture, double bubble appearance, ALCL, risks associated with general anaesthetic, blood clots in legs or lungs.
“From the initial, free, consultation through to the final post-op checkup, Mr Mahajan’s professionalism has been exemplory. He answered my many doubts and questions with unbiased and down to earth advice, and patiently explained every option and procedure open to me. The operation and subsequent recovery were without any problems, and as far as I can see he has left me with absolutly no obvious scarring. I do not hesitate in recommending Mr Mahajan to anyone considering facial surgery.”
“I spent a substantial amount of time researching potential options and considering the merits of each before deciding to go with Mr Mahajan. It was the best decision I could have made, the results of the surgery were far beyond what I ever thought possible. Mr Mahajan is a perfectionist but one who makes it clear just what is achievable with surgery. In my opinion, Mr Mahajan is, without any…”
Mr Mahajan will acquire a detailed history from you about your concerns and your medical history. He will take the time to understand your desires and discuss in details as to how he can achieve the results you want. A detailed examination involving assessment of the breast tissue and overlying skin envelope in relation to your chest and physique will be noted. Measurements will be taken to gauge the degree of the problem and any asymmetry.
Depending on your examination a treatment plan will be formulated tailored to your needs. If you are not happy with the volume of your breasts in an unpadded bra and your breasts are droopy and empty then an breast augmentation mastopexy procedure will help achieve the results you aspire for. If your only have a mild droop to your breasts and want to go bigger, then an implant on its own might be enough to uplift the breasts, avoiding the additional scars that go with a full breast uplift procedure. Mr Mahajan feels that your breasts should ideally be of a volume that suits your chest. The planned procedure will be tailored to your specific requirement. Pattern of the incisions, procedure and subsequent scars will be discussed in detail and you will be given an opportunity to probe into any aspect of the proposed procedure.
Once you decide to go ahead following the consultation, you will be required to attend the pre-assessment clinic to ensure you suitability for the procedure under general anaesthetic. It is not considered safe to carry out a breast augmentation mastopey procedure in a patient who is a smoker or has a very high BMI.
Operation
You will be admitted to the hospital on the day of the procedure. The operation will be done under general anaesthesia. It will be carried out according to the technique that was planned at the consultation. This will depend on the characteristics of your breast and will involve using the vertical scar, the wise pattern or periareolar or minimal scar technique.
In large breast uplifts, Mr Mahajan prefers to use his innovated version of the wise pattern technique that helps him achieve very good results as desired by the patient. The procedure will be tailored to your requirement and scars will be kept to a minimum as required. The procedure may need to be combined with liposuction if there is significant fullness of the lateral chest wall. This can be discussed at the consultation prior to the procedure. The procedure can take 3 to 4 hours to do depending on the complexity of the case. Mr Mahajan will dedicate as much time as is necessary to mould the breast tissue into their new aesthetically pleasing form and achieve the results you desire.
Following your procedure, you will be taken to your room once you have recovered from the anaesthetic. You will be cared for to the highest standards by our well-trained nurses. Once you have recovered enough after the surgery, you will be encouraged to sit out of the bed and mobilise to reduce the risks of blood clots in your legs or lungs. You will have some pain and discomfort for 3 to 7 days, but we will ensure that you are comfortable will adequate analgesia. You will have drains in that will come out in one to three days depending on the drainage.
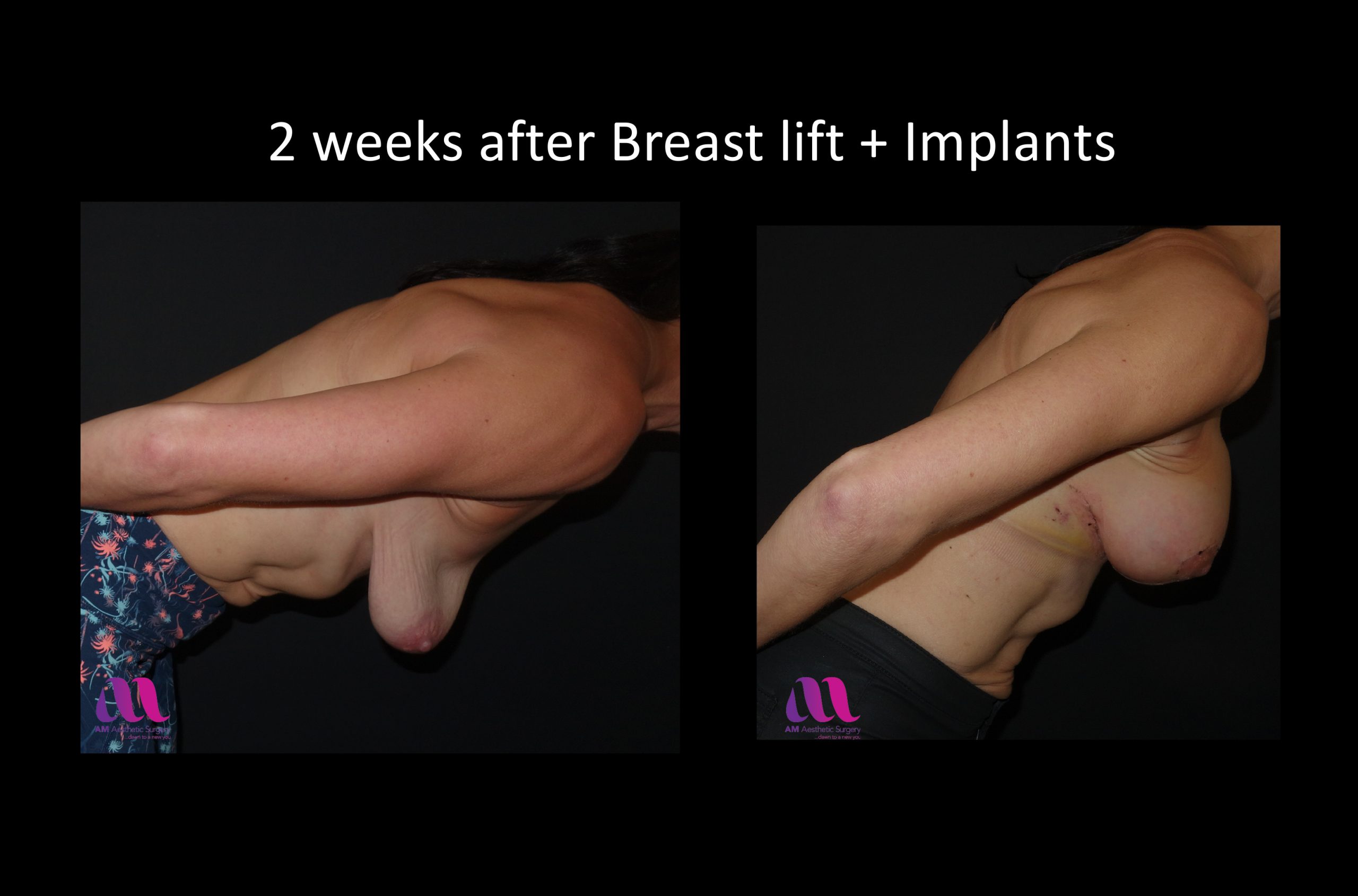
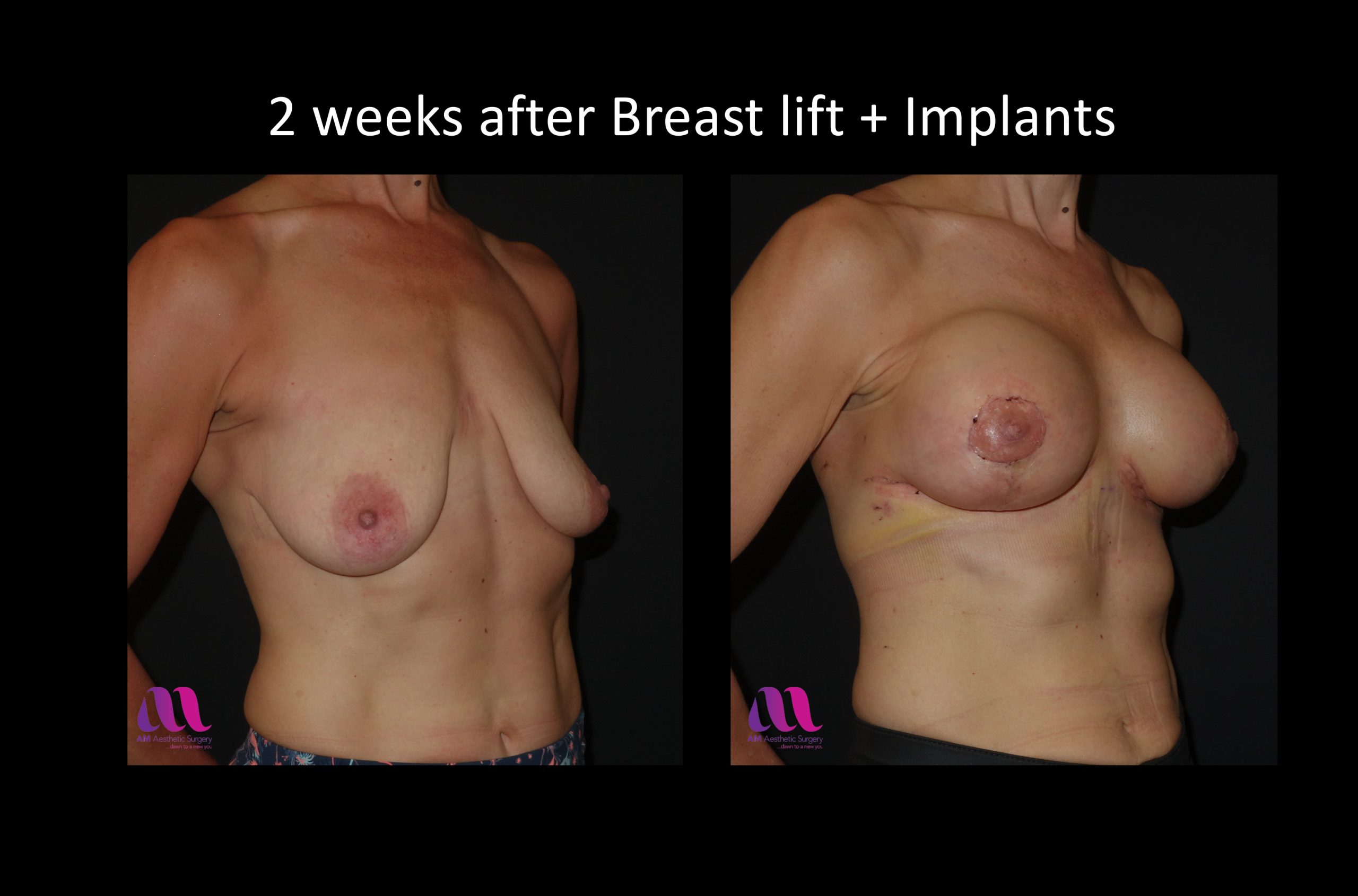
You can go home as soon as the drains have been removed and you are feeling well enough to go home. You will have dissolvable sutures and as a result you will not need to endure the discomfort of them being removed and also this will prevent you from getting any stich marks around your scars. Scars are unavoidable following any surgery, but Mr Mahajan aims to make these as neat as possible. Your breasts will be swollen, tense and appear prominent immediately following the surgery. Over the next few months the swelling will gradually go down and the breast will assume a more natural ptotic position. You are advised to wear a sports bra for 2 to 3 months. Once the swelling has decreased in 3 months or so you can consider investing in new lingerie!
You will be seen 2 weeks following the procedure to ensure that your wounds have healed well. After this initial follow up, you will be seen again in 3 months’ time to assess the results when the swelling has settled reasonably. Mr Mahajan will be available to see you at any time following the procedure should there be any unexpected problem.
Is breast augmentation mastopexy for me?
If you have lost significant weight, if pregnancies have been unkind to you and you have ended up with empty, droopy or saggy breasts that are out of shape, you will benefit from a breast augmentation mastopexy procedure.
What is the most important consideration prior to deciding to have a breast augmentation mastopexy procedure?
Experience and extensive studies have shown us that breast implants are safe. However, patients do need to appreciate that breast augmentation may not be a once off procedure and you may need to be operated upon again in future. This may be many years down the line, if you have a problem. There will be scars following the surgery and one has to be accepting of these, but if you can accept this trade off for much more shapely breasts then you would have made the right decision. Most of Mr Mahajan’s patients comment upon how the augmentation mastopexy has helped boost their confidence and changed their lives.
How do I know if my surgeon is qualified in the field of Plastic Surgery?
MB BS, MB BCh or MB ChB is the basic medical degree of any doctor. Your plastic ‘surgeon’ should at least be a ‘surgeon’. Doctors who receive adequate ‘basic’ surgical training in the UK are awarded Fellowship (FRCSI, FRCS, FRCS Ed, FRCS Gl – in the older generation of surgeons) or Membership (MRCS – in the younger generation of surgeons) of the Royal Colleges in the UK. Doctors or Surgeons, who believe in having a scientific foundation to their practice, spend further years doing research in their fields and are awarded Research degrees such as MSc, MMedSc, MPhil, MD or PhD. Surgeons who ‘train specifically in the field of Plastic surgery’ are awarded FRCS (Plast). These surgeons are then entitled to be on the “Specialist register for Plastic Surgery” with the General Medical Council (GMC).
How do I choose amongst the Plastic Surgeons who fit the above criteria?
‘Safe’ and ‘beautiful’ results are dependent on ‘experience’ and ‘expertise’ of your plastic surgeon. Mr Mahajan is a highly trained and experienced plastic surgeon who is a Consultant Plastic Surgeon at the Bradford Teaching Hospitals NHS Foundation Trust / Calderdale and Huddersfield NHS Foundation Trust and is the Director of the prestigious Plastic Surgery and Burns Research Unit (PSBRU) at the University of Bradford. He believes in practising “evidence based medicine” by engaging in research activities to help establish a scientific background to his / her clincial practice. He has a specialist interest in Breast surgery having worked in world-renowned centres for breast surgery in Belgium, Sweden and Switzerland in addition to his training in the UK. It obviuolsy helps if your surgeon has travelled the world to enhance his training in premier institutes to learn from leading surgeons in their fields. He is a full member of the British Association of Plastic Surgeons (BAPRAS), British Association of Aesthetic Plastic Surgeons (BAAPS), European Association of Plastic Surgeons (EURAPS), UK Association of Aesthetic Plastic Surgeons (UKAAPS), American Society of Plastic Surgeons (ASPS), Association of Breast Surgeons (ABS) and is on the Specialist register for plastic surgery with the General Medical Council (GMC). Surgeons are only awarded membership of these associations if they are properly qualified and it is a reassurance for you that you are in safe hands.
Where will my surgery take place?
Your surgery will take place in ‘local’ reputed hospitals such as the Yorkshire Clinic or the Spire Elland Hospital, where you will be able to return to ‘anytime’ after the operation should there be any concerns.
How much will the procedure cost?
Cost of breast uplift can be about £7500 depending on the procedure you need. Mr Mahajan will discuss this with you when you meet him. You may find cheaper deals with firms that consider cosmetic procedures as a business, but may end up compromising on safety, quality and convenience. Although breast uplift is considered as a cosmetic procedure, it is a plastic surgical ‘operation’ and you do need to appreciate this and consider it with all the seriousness that it deserves. Medical tourism has certainly made costs cheaper, but the very fact that you are boarding a long haul flight puts you at risk of blood clots in your legs or lungs that can be life threatening. There are obviously other matters to consider such as qualifications, experience as expertise of your surgeon / anaesthetist apart from the ability to see your surgeon again should there be a problem and you have flown back home.
How will a breast augmentation mastopexy procedure help me?
The breast will have a increased volume with a nice aesthetically pleasing shape to them with appropriately sized areola. The will be proud of your new wardrobe! The breasts will be proportionate to your body. It will help relieve any episodes of rashes under the breasts. Your self-esteem will be hugely elevated and your breasts will no longer lie in your arm pits when lying down in bed!
Will I have scars?
Scars are unavoidable following any surgery, but Mr Mahajan aims to make these as neat as possible. You will either have a wise pattern (inverted ‘T’ / Anchor pattern) or vertical (lollipop scar) or periareolar or infra mammary scar.
Will my scars be visible?
The standard wise pattern or key hole pattern or inverted ‘T’ or anchor pattern incision results in scars around the circumference of the areola, a scar running along the crease under the breast and a vertical scar extending from the areola to the crease. The scar in the crease tends to be tucked away, the scar around the areola is not very conspicuous as the areolar skin tends to different from the breast skin, part of the vertical scar that is not tucked away under the breast is the most prominent part of the scar. In a vertical scar breast reduction procedure the scar is around the areola and vertical down from it to the breast crease. In a periareolar technique, the scar will only be around the areola. In a minimal scar technique, the scar will only be in your crease and is tucked away under the breasts.
Is there a difference in quality of the scars between the different techniques used?
Although patient prefer to have short scar techniques such as the vertical scar or the periareolar scar techniques, the scar can be thicker, crinkled and wider in these procedures as the skin is bunched up when suturing it together to keep the length of the scar down. This can result in a flattened appearance of the breast in the lower or central part of the breast depending on the technique used. A wise pattern scar allows the best possible redraping of your breast tissue, although at the expense of longer scars.
How will my breasts be affected by the augmentation mastopexy?
Excess skin will be removed resulting in tightening up of the skin envelope with the enhanced breasts looking more shapely and pert. Your nipples will be lifted up to the appropriate position on your newly shaped breasts.
Is the nipple removed in a breast augmentation mastopexy procedure?
The nipple is not removed in breast uplift procedures, it is only moved up to where it belongs.
What type of Implants do you use?
Mr Mahajan uses both silicone gel and saline implants according to the patient’s wishes. However, most patients choose to have silicone gel implants as they tend to feel more natural and maintain a better shape. You can have an anatomical or tear drop shaped implant or a round implant. Details of these will be discussed with you at your consultation. Mr Mahajan only uses implants that have a good track record and has never used PIP implants. The PIP implants contained non-medical grade silicone to be sold at a cheap price and used by some of the clinics that treat cosmetic surgery purely as a business. Mr Mahajan strongly believes that if something is being provided at a significantly reduced cost, there has to be a reason for it that may not necessarily be in the best interest of his patients.
How do I select my implant?
At your consultation, Mr Mahajan will explain the difference between various kinds of implants. You will have the opportunity to see and feel the implants. Together, you can decide the type of implant that is right for you once you have informed knowledge about them. Mr Mahajan will do a detailed examination of your chest and take some measurements. Using the Biodynamic breast analysis system, he will be able to guide you to select implants that are suitable for your chest and you can pick amongst these.
Do you use smooth walled or textured wall implants?
Professor Mahajan uses both textured and smooth wall implants. It is believed that there is a decreased incidence of capsular contracture with textured implants. Moreover, the textured surface helps tissue around the implant to integrate into the surface of the implant and prevents the implant from rotating which can potentially happen in a shaped implant. Textured implants have however been associated with ALCL (Lymphoma – cancer). There have been some cases of ALCL reported in smooth implants as well, but these may have been associated with use of other implants prior to use of the smooth implant. For detailed information on ALCL, please look at information about ALCL in this section.
What size will my breasts be after the procedure?
Following a detailed examination and consultation, you can discuss with Mr Mahajan and plan as to what size you would like your breasts to be. Whilst it is nice to have larger boobs, it is equally important for them to look as natural as possible. As a general rule, the larger the implant, the harder it is to hide them. The volume of the implant is dictated by your breast base diameter. Ideally your implant should be placed within the confines of your breast base to give you a naturally augmented result. Mr Mahajan can guide you with this after he has examined you and taken detailed measurements. One should also take in to account the weight of the implants. The larger the implants, the heavier they will be and this can stretch down your breast envelope with time and make them droopy again. Ideally your breasts should be of a size that suits your chest.
When will I need my implants changed?
Implants do not need to be changed unless there is a problem with your augmentation. More often revision surgery is not for changing a ruptured implant. You do not need revision surgery unless, you have a problem with capsular contracture, droopy breasts with time and age, desire for change in size of breasts or other such reason. Even if your implant is ruptured, the silicone is still contained in the capsule that your body forms around the implant. At times you can have extra capsular ruptures that can result in silicone deposits in your breast tissue or lymph nodes in your axilla. This is not supposed to be harmful, but can at times be uncomfortable. If there are obvious signs of a ruptured implant with change in shape of the breast, it is recommended to have them replaced.
Do silicone breast implants increase my risk for breast cancer or autoimmune disease?
There have been extensive studies done on this topic and an Independent review group in the UK (1998) has found silicone breast implants are not associated with a greater health risk when compared to other surgical implants.
Can I breast feed if I have had breast implant?
Yes you can, it has been shown that cow’s milk and infant formulas contain a higher level of silica than breast milk from women with silicone implants.
What is ALCL and what are my risks of developing it?
Anaplastic large cell lymphoma (ALCL) is a rare type of non-Hodgkin lymphoma (NHL), a cancer involving the cells of the immune system. ALCL in the breast is rare.
Textured implants have been preferred over the years to reduce incidence of capsular contracture and to prevent the implant from rotation in anatomical (tea drop shaped) implants. Shaped implants are better in providing as natural (anatomical) shape as possible to the augmented breast especially in patients who have very little of their own breast / subcutaneous tissue.
Patients do need to be fully aware that there is a risk of ALCL associated with any breast implant but the risk is low. Although most cases are associated with textured implants, there are cases associated with smooth implants too, but some of these cases have a history of previous textured implants. Cases have been reported from most manufacturers and not a particular brand of implant. Although ALCL is a type of cancer (lymphoma), it is not breast cancer and is mostly treatable. Patients who have breast implants do not have to have them removed, but they do need to be vigilant of signs and symptoms that may reflect underlying problems.
For details please refer to the following credible sources.
BAAPS
//baaps.org.uk/patients/safety_in_surgery/breast_implant_safety.aspx
“The British Association of Aesthetic Plastic Surgeons advises that concerned patients need not take any action at this stage. They should continue their routine follow up with their healthcare professional and discuss any questions they have about their breast implants. There is no need to remove or exchange any current implants based on the most up-to-date scientific data available. Indeed, unnecessary surgery may cause additional harm in a small number of patients.”
Breast implants safety – statement issued by
The Association of Breast Surgery (ABS)
The British Association of Aesthetic Plastic Surgeons (BAAPS)
The British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS)
“The consortium of journalists has highlighted the known link between breast implants that have a textured surface and the condition Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). BIA-ALCL is rare and, usually, eminently treatable. (Statement available here) Current research suggests the risk of developing this condition in the UK is approximately 1 in 24,000 breast implants sold. Not all textured surfaces are manufactured in the same way and they appear to convey different levels of risk, hence it is difficult to draw definite conclusions about the type of texturing at this time. Texturing of an implant surface however conveys advantages over smooth implants, particularly with more naturally shaped implants. Hence many surgeons in the UK still advocate the use of textured implants for their patients. It is vital however, that the risks of using textured or smooth surfaced implants are fully discussed with all patients before surgery so that they are able to make fully informed choices.”
BAPRAS
//www.bapras.org.uk/professionals/clinical-guidance/alcl-risk-from-breast-implants
“BIA-ALCL appears to be related to textured breast implants and it appears to have occurred with textured implants made by every manufacturer.”
“BIA-ALCL is a lymphoma and not cancer of the breast tissue. When breast implants are placed in the body, they are inserted behind the breast tissue or under the chest muscle. Over time, a fibrous scar called a capsule develops around the implant, separating it from the rest of the breast. In women with breast implants, the ALCL was generally found adjacent to the implant itself and contained within the fibrous capsule.”
MRHA
//www.gov.uk/guidance/breast-implants-and-anaplastic-large-cell-lymphoma-alcl
“In the UK, the estimated risk of BIA-ALCL, based on the reported confirmed cases is 1 per 24,000 implants sold. This estimate is based on data for all types of breast implants known to be sold in the UK and reported cases of BIA-ALCL confirmed to meet the WHO criteria until July 2018.”
FDA
“risk of developing BIA-ALCL for a woman with textured implants is 1:3,817 to 1:30,000”
“Most confirmed cases of BIA-ALCL have occurred in patients with textured-surface implants, although there are known cases in patients with only smooth-surface implants.”
“The FDA update calls for no changes in recommendations regarding breast implants. For patients with breast implants, the FDA states there is no need to change routine medical care and follow- up, and there is no need to test asymptomatic patients.”
ASPS
//www.plasticsurgery.org/for-medical-professionals/health-policy/bia-alcl-physician-resources
“Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) is an uncommon and highly treatable type of lymphoma that can develop around breast implants. BIA-ALCL occurs most frequently in patients who have breast implants with textured surfaces.
The current lifetime risk of BIA-ALCL is estimated to be 1:3817 – 1:30,000 women with textured implants based upon current confirmed cases and textured implant sales data over the past two decades. Since the initial case report in 1996, ASPS now recognizes approximately 265 cases in the US and a total of 688 worldwide as of February 8, 2019.
Most of the patients who have developed BIA-ALCL receive an excellent prognosis following surgical removal of the breast implants and the surrounding scar tissue capsule. Continued follow-up after any breast implant surgery is suggested and important for patient health, but patients who notice pain, lumps, swelling, fluid collections or unexpected changes in breast shape, including asymmetry, should contact their plastic surgeon. In most cases, women diagnosed with BIA-ALCL observed changes in the look or feel of the area surrounding the implant greater than one year after their initial surgical sites were fully healed, and on average eight to ten years after receiving textured implants.”
What is Breast Implant Illness (BII)?
Some patients experience symptoms such as tiredness, “brain fog”, joint aches, immune-related symptoms, sleep disturbance, depression, hormonal issues, headaches, hair loss, chills, rash and neurological issues which may be associated with breast implants. To date there is no scientific explanation for this and there is no proven link between developing these symptoms and having breast implants, but we cannot ignore the fact that some patients have claimed that their symptoms have got better on removal of their implants. Patients opting to have breast implants need to aware of the risks of Breast Implant Illness (BII).
For further information about breast implant illness (BII) please refer to the following websites.
//www.gov.uk/guidance/symptoms-sometimes-referred-to-as-breast-implant-illness
//baaps.org.uk/_userfiles/pages/files/bii_information.pdf
//www.fda.gov/medical-devices/breast-implants/risks-and-complications-breast-implants
//www.surgery.org/sites/default/files/downloads/BII-Talking-Points-FINAL-1.15.19.pdf
What is capsular contracture?
When any object foreign to the body is placed inside the body, the body tends to wall it off by forming a envelope around it. This is called a capsule. Everyone one gets a grade one capsule, which is the normal reaction of the body. It is made up of contractile tissue that can potentially contract with time, making the envelope around the implant smaller. This can result in you being able to feel the implant and capsule (grade 2 capsule). If the contraction progresses and the envelope becomes even smaller, then the implant may start to look like a round ball and this can result in change in shape of the augmented breast (grade 3 capsule). With further progression, capsular contraction can start becoming uncomfortable (grade 4 capsule). It is hard to predict the chances of you developing an adverse capsule and this varies greatly amongst patients. There is nothing you can do to prevent this from happening. Meticulous surgical technique does help and Mr Mahajan takes care and time to do the surgery as safe as possible for you. If are unfortunate enough to develop a bad capsule, then you may need revision surgery in future.
What is double bubble appearance?
With breast augmentation, your implants may end up staying in their pockets where they were placed (first bubble). But with time, age and gravity, your natural breast tissue may sag and droop below the level of your implants, causing the appearance of a second bubble. You may need revision surgery to improve on this appearance in future… should you develop it.
Will my implants be in front of the muscle or behind it?
The implant can be placed in a subglandular, submuscular or dual plane pocket. The subglandular plane involves dissecting the pocket for the implant under the gland, but over the muscle. This plane can be used in patients who are not keen on having the implant placed under the muscle as they have a very physical job. Recovery can also be a few days quicker with the approach. However, you need to have a minimum amount of breast tissue to be able to hide the implant (this will be assessed at the time of your consultation with Mr Mahajan). The pocket is dissected under the muscle in a submuscular plane, which results in the muscle giving some added cover over the implant, making it less visible and palpable. There can however be issues with movement of the implant (animation of the implant), with contractions of the muscle. It will also result in some degree of weakening of your pectoral muscle, but there are two pectoral muscles (major and minor) and the implant is placed below the Pectoralis major, leaving the Pectoralis minor intact. Mr Mahajan prefers to use the dual plane technique which is a combination of the placing the implant below the muscle and the gland. In a dual plane technique, the pocket is dissected below the Pectoralis major muscle, but the muscle is released in the lower part, reducing the risk of animation of the implant. A plane is also dissected above the muscle to a varying degree (dual plane 1 to 3) according to the nature of your breasts. This helps redrape the breast envelope appropriately over the newly enhanced volume of your breasts. The implant is covered by both the breast gland and the muscle in the upper part and is less prone to be visible and palpable. The muscle does not cover the lower outer part of the implant, where it is covered by your own breast and subcutaneous tissue. A dual plane breast augmentation tends to give the best possible result as advocated by gurus of breast augmentation surgery, Dr John Tebbets and Dr Per Heden. Mr Mahajan has had the opportunity to train and master his breast surgical skills with Dr Heden during his period in Stockholm.
Will my augmented breasts look natural?
Your breasts will have a naturally augmented look if you select the right implant (with guidance from Mr Mahajan). A natural aesthetic breast tends to have a gentle slope in the upper part, peaking at the nipple and a rounded lower part of the breast. This can be achieved by using a natural shaped or anatomical shaped or tear drop shaped implant. It is important to select an implant that sits within the confines of the foot print of your breast and suits your chest wall. Generally speaking, the larger the implant, the more the risk of an unnatural result. A large implant can result in a rounded appearance in the upper pole, rather than a gentle slope. But if this is what you desire, then this is what you may need to go for.
Will my breasts be round and full in the upper part?
This depends on your personal choice. If this is the look you would want to acquire, then it can be achieved with the use of round implants or large shaped implants. There is risk that your breasts may look a bit fake. But it is important that you are happy with the outcome of the surgery after having spent all that money and if this the look you want to achieve, then you should clearly express this.
Will my nipples be less sensitive?
Sensation to the nipple and the skin can be altered following a breast augmentation mastopexy procedure. The sensation may not change, but can be decreased to some extent. At times the nipples can end up being hyper sensitive.
Will the procedure affect my mammograms in future?
Mammograms are not affected following a breast augmentation procedure. There might be some signs of scarring. A different technique can be used to do mammograms in the presence of an implant and if there is a problem with the mammogram, an MRI scan can be performed.
Will the procedure affect my ability to breastfeed?
Not necessarily. During a breast augmentation procedure, the implant is placed under your breast gland (either under the gland itself or under the muscle, which is under the gland). This does not disrupt the milk ducts from the gland to the nipple, unless a trans areolar approach is used. However, larger implants can put pressure on the breast gland and result in pressure atrophy or reduction of the breast gland, which can potentially affect the amount of milk produced.
Will fluctuations in weight affect the appearance of my breasts?
Your breast and subcutaneous tissue that can fluctuate in volume with hormones and changes in bodyweight. Also, the uplifted breasts will droop down slightly as the initial swelling settles down. In other words, the breasts will change in appearance, as natural breasts would do. If you gain significant amount of weight, the breast may become more heavy and have a tendency to be more droopy with time.
Will my augmentation mastopexy be done in one operation or two?
Some surgeons prefer to do the breast augmentation in the first operation followed by a mastopexy at a second operation or vice versa. Dr Per Heden of Akademikliniken in Stockholm is renowned for his technique of doing breast augmentation mastopexy in a single operation. He conducts master classes for surgeons across the world to teach his technique. Mr Mahajan has had the opportunity to train with him during his period in Stockholm and is happy to do the procedure in a single operation. An augmentation mastopexy can be carried out safely as a single operation by using the right technique, negating the need for a second general anaesthetic and its added costs.
Is a breast augmentation mastopexy permanent?
During a breast uplift procedure, the skin envelope is tightened and the nipple is elevated. The position of the nipples will not droop down again significantly. They might go slightly lower as the swelling settles. However, it is known that the distance between the nipple and the crease under the breast can increase with time, with the effects of gravity. This depends on the elasticity of the skin and the weight of the breast tissue/implant. This can be revised in future if necessary.
Do I need to stop my medication?
If you are on the oral contraceptive pill, you will need to stop these 4 weeks before the procedure to reduce your risks of blood clots in legs or lungs. Also, you will need to stop any blood thinning drugs. Aspirin and Clopidogrel will need to be stopped a week prior to surgery. Warfarin, Dabigatran etexilate, Rivaroxaban and Apixaban need to be stopped 4 days prior to surgery. Mr Mahajan will discuss this with you in the pre operative consultation.
Will I need to have a general anaesthetic?
Yes, you will need a general anaesthetic to undergo the procedure. It will take about 3 to 4 hours to do the operation for you. Your anaesthetist will be fully qualified and a member of the Royal college of Anaesthetists. He will ensure that you have a smooth anaesthetic procedure and are comfortable during your recovery.
Are there any risks?
Every effort is made to reduce the risk of complications, but potential risks are bleeding, bruising, swelling, haematoma / seroma, infection, explantation of the implant, delayed wound healing, scars – hypertrophic, stretched, sensitive, not in the inframammary crease, no guarantee of cup size or cleavage, altered sensation – decreased or increased, altered lactation and mammogram, asymmetry, nipple loss, fat necrosis, Implant – visibility, palpability, rippling, rotation, rupture, silicone granuloma / axillary lymphadenopathy, capsular contracture, double bubble appearance, ALCL, risks associated with general anaesthetic, blood clots in legs or lungs.
How long will I have to stay in the hospital?
You will have surgical drains after the procedure and will need to stay in for 1 to 3 days depending on the drainage. You will be discharged only when you are comfortable enough to go home.
How long will it take for my wounds to heal?
It takes about two weeks for the wounds to heal up. At times, wound healing can be delayed at the ‘T’ junctions of the wounds where the blood supply is the least and tension is the most. You will need dressings until the wounds are healed in two weeks, but if wound healing is delayed is some areas, you will need dressings here until the wounds are fully healed.
When can I shower or have a bath?
You should ideally wait for two weeks until your wounds are healed and dressing are removed before you have a bath. However, you can wash yourself and have a sponge bath keeping the dressing dry as soon as you are able to.
How long will it take for my scars to settle?
Scars tend to settle reasonably in 3 to 6 months. However, it takes about 12 to 18 months for scars to settle fully. Scars can at times be thickened (hypertrophic) especially in younger patients. This might require treatment with silicone creams or steroid injections.
When can I sun bathe?
It is always advisable to protect your skin in the sun. In particular, your new scars are susceptible to sun damage until they mature in about a years’ time or so. You should keep the scars covered or protected with a high factor sun protection cream until then.
What can I apply to my scars to help them settle better?
It is important to massage the scars once they are healed. This helps them settle better. Some patients claim that Bio oil helps scars settle better, but any moisturising cream should be good enough. If there is any indication of the scars becoming thicker, then silicone based creams should be considered.
When will I be seen again after I am discharged from the hospital?
You will usually be seen by Mr Mahajan 2 weeks following your procedure to ensure that the wounds have healed well. Following this initial review, you will be seen again in 3 months. However, if there are any concerns, you will be seen by Mr Mahajan as often as is necessary.
Is there any thing that I need to look out for?
Although you will only be discharged from the hospital when Mr Mahajan is satisfied that you doing well following your surgery, you do need to look out for sudden increase in swelling of the breast, disproportionate pain, any signs of infection such as feeling unwell, temperature, redness around the scars, discharge or foul odour from the wounds. Your nipples can be a bit bruised after the procedure, but should their colour change to purple or pale, it could be sign of compromised circulation and you should return to see Mr Mahajan.
Will I need to wear any special garments?
You will need to wear a lycra sports support bra that is not underwired following the procedure. My Mahajan will discuss the potential bra size with you during your preoperative consultation. It would be ideal to wear this for about eight to twelve weeks following the procedure. As the swelling goes down after this period you can invest in a new wardrobe of lingerie.
Will I be in pain?
Patients do tend to have some pain and discomfort for the first 1 to 3 days, but you will be kept comfortable with adequate analgesia. It is advisable to take Paracetamol six hourly on a regular basis for the first 24 to 48 hours and then as necessary after that.
Will my breasts be swollen?
Your breast will indeed be swollen immediately after the procedure. The swelling takes time to settle and it will be significantly less a month following the procedure. It takes about three months for it to settle reasonably. It continues to further settle gradually after that and can take up to a year for the end result to be apparent
Will my breast be bruised?
There will be some bruising present especially adjacent to the scars. This will gradually settle over in two to three weeks.
Will I be in pain?
Patients do tend to have some pain and discomfort for the first 1 to 3 days, but you will be kept comfortable with adequate analgesia. It is advisable to take Paracetamol six hourly on a regular basis for the first 24 to 48 hours and then as necessary after that.
When do my stitches come out?
Mr Mahajan uses absorbable sutures to close the wounds. This helps him achieve neat scars and prevent ‘hatch marks’ from external sutures. This also means that you will not have the discomfort of having your sutures removed.
What if I have a problem after I am discharged from the hospital?
You will be discharged from the hospital when it is safe enough to do so. However, in the event of any unexpected problems, you can contact us any time on 0800 246 5636.
What position can I sleep in?
You will be most comfortable lying on your back immediately after your surgery. After your surgery, the breast implant becomes surrounded by a capsule (or envelope). In the first four to six weeks the position of this capsule can be influenced by outside forces such as activity, sleeping position, and bra support. I would recommend that you sleep on your back for four to six weeks so that outside forces do not influence the formation of scar tissue around your implants. Sleeping on our side while wearing the support bra is okay, if you are more comfortable sleeping on your side. But I would not recommend sleeping on your tummy for six weeks.
When can I go back to work?
This depends on your job. If you have a desk job that does not involve lifting any things heavy, you can go back to work as soon as you are comfortable and this could be as early as 5 days to two weeks. However, if you have a more demanding job, you will need to take a break for four to 6 weeks. This can vary widely between patients, as patients tend to cope variably.
When can I pick up my baby?
You can lift your baby up as soon as you are comfortable to do so. This can be towards the end of the first week. But you do need to careful that you don’t strain yourself. Alternatively, your partner could give the baby to you to hold gently. Do not try to restrain an aggressive child as you would harm yourself.
When can I hit the gym again?
You will need to wait until your wounds have fully healed and you are comfortable to under take any labour intensive work. This could take 4 to 6 weeks following your surgery. You could however return to light cardiac exercises sooner in about 2 to 3 weeks.
When can I drive?
You will need to wait until you are comfortable to do so. This might mean waiting till your wounds have healed in two weeks time. You should be able to apply an emergency stop and it is a decision that you will have to make.
When can I fly or go on holidays?
Holidays after surgery will do you good and give you time to recuperate. However, it is not advisable to go on long haul flights for 4 weeks after the procedure to reduce the risks of blood clots in your legs or lungs. Blood clots in your lungs can be life threatening and is a very compelling reason for you not to consider traveling across the globe in search of cheap deals. Short flights and travel by train or car, which does not involve prolonged periods of immobilisation, is not a problem although you should take precautions to wear flight socks when travelling.
Although I am not in any rush, when can I have sex again?!
You will need to wait until your wounds have fully healed and you are comfortable to engage in any sexual activity. This could take 4 to 6 weeks following your surgery. You certainly need to be careful for at least 2 weeks until the wounds have healed.
When can I drink or smoke?
There is no issue with having a social drink after the procedure. However, patients do need to refrain from smoking completely for at least three weeks following the procedure. You would have had to stop smoking for eight weeks before the operation. Smoking tends to reduce the circulation of blood, which is vital for wound healing. This applies to nicotine patches or electronic cigarettes too. Considering that you would have stopped smoking for about 3 months around the date of your procedure, you should take this as an opportunity to stop smoking completely!
Book chapters:
Principles of free flap design and elevation
Phillip N Blondeel and Ajay L Mahajan
Operative Microsurgery, edited by Brian Boyd, MD and Neil Jones, MD. McGraw-Hill, New York, 2015.
Microsurgical Breast Reconstruction in Presence of Co-morbidities
Seidenstuecker, Katrin; Munder, Beatrix; Mahajan, Ajay L; Andree, Christoph
Breast Reconstruction; Art, Science, and New Clinical Techniques, edited by Shiffman, Melvin A. Springer, Switzerland 2015
Photography in Plastic Surgery
Ajay L Mahajan
Text Book of Plastic, Reconstructive & Aesthetic Surgery, edited by Karoon Agarwal, in Print
Articles:
- DIEAP flap for safe definitive autologous breast reconstruction
Seidenstuecker K, van Waes C, Munder BI, Claes KEY, Witzel C, Roche n, Stillaert F, Mahajan AL, Andree C, Blondeel PN
Breast 2015.12.005 - Morbidity of microsurgical breast reconstruction in patients with co-morbid conditions
Seidenstuecker K, Munder B, Mahajan A L, Andree C
Plast Reconstr Surg. 2011 Mar;127(3):1086-92. - Are Pfannenstiel scars a boon or a curse for DIEP flap breast reconstructions?
A L Mahajan, A Zeltzer, K E Y Claes, K Van Landuyt, M Hamdi
Plast Reconstr Surg. 2012 Apr;129(4):797-805. - Myosonographic Study of Abdominal Wall Dynamics to Assess Donor Site Morbidity after Microsurgical Breast Reconstruction with a DIEAP or ms-2 TRAM Flap
K Seidenstücker, B Munder, P Richrath, U Legler, A L Mahajan, C Andree
JPRAS in print - DIEAP flap for safe definitive autologous breast reconstruction
Katrin Seidenstuecker, Carl van Waes, Beatrix I Munder, Karel E Y Claes, Christian Witzel1, Nathalie Roche, Filip Stillaert, Ajay L Mahajan, Christoph Andree, Phillip N Blondeel
The Breast in print - The ECG dot as a pre operative marker for Nipple Areolar Reconstruction
A L Mahajan, A J Hussey, C L Riordan, P J Regan
Plast Reconstr Surg. 2003 Feb;111(2):955 - Preventing ‘T’ junction dehiscence in mammaplasty
AL Mahajan, TWL Chapman, JG McDiarmid
Plast Reconstr Surg. 2006 May;117(6):2100. - Radiotherapy tattoo – a landmark for an underlying expander implant port in breast reconstruction
VA Mahajan, AL Mahajan, Morris RJ
J Plast Reconstr Aesthet Surg . 2010 Feb;63(2):e171. Epub 2009 Apr 5. - Attaining symmetry in breast reconstruction procedures
J K Dickson, J M Taylor, R Rajan, A L Mahajan
J Plast Reconstr Aesthet Surg 2010 Sept; 63(9): 1573-1575. Epub 2010 Mar 10. - Pectoralis fascia grafts in breast reconstruction.
Gran MV, Nicholson S, Mahajan AL.
J Plast Reconstr Aesthet Surg. 2012 Apr;65(4):e104-5 - The inferior based pectoralis fascial flap for breast reconstruction.
Mahajan AL.
J Plast Reconstr Aesthet Surg. 2012 Nov;65(11):1599-601 - Breast Equalising Surgery following Breast Reconstruction
A L Mahajan, L Rynn, A Grufferty, P J Regan
Ir J Med Sci. 2002 July/Aug/Sept 171(3) S2: 21 - Sun burn from resting reading glasses on a reconstructed breast!
AL Mahajan, TWL Chapman, M Mandalia, RJ Morris
J Plast Reconstr Aesthet Surg. 2010 Feb;63(2):e170. Epub 2009 Jun 7. - The Safety of the Deep Inferior Epigastric Artery Perforator Flap Procedure: A Prospective Analysis in 1036 Breast Reconstruction Patients.
Waes, Carl Van; Seidenstuecker, Katrin; Mahajan, Ajay; Roche, Nathalie; Stillaert, Filip; Andree, Christoph; PN Blondeel.
Plast Reconstr Surg. 128(4S):57, October 2011.
Presentations:
- Breast Equalising Surgery following Breast Reconstruction
A L Mahajan, L Rynn, A Grufferty, P J Regan
Sir Peter Freyer Meeting, Galway, September 2002 - Sun burn from resting reading glasses on a reconstructed breast!
AL Mahajan, Chapman TWL, M Mandalia, Morris RJ
Irish Association. of Plastic Surgeons Meeting, Galway, May 2007 (Poster presentation) - ‘Custom made’ DIEP flap breast reconstructions
A L Mahajan, R Rajan, A P Tregaskiss, A Perez, R J Morris
Irish Association. of Plastic Surgeons Meeting, Galway, May 2009 - Attaining symmetry in breast reconstruction procedures
J K Dickson, J M Taylor, R Rajan, A L Mahajan
Irish Association. of Plastic Surgeons Meeting, Galway, May 2009 (Poster presentation) - Attaining symmetry in breast reconstruction procedures
J K Dickson, J M Taylor, R Rajan, A L Mahajan
XXXIVth Sir Peter Freyer Surgical Symposium meeting, Galway, Ireland, Sept 2009. (Poster presentation) - Attaining symmetry in breast reconstruction procedures
J K Dickson, J M Taylor, R Rajan, A L Mahajan
International Plastic Reconstructive & Aesthetic Surgeons meeting, Delhi, Nov 2009 - Creating a template of the contralateral breast to aid DIEP flap reconstruction.
R Rajan, A P Tregaskiss, A Perez, A L Mahajan, R J Morris
International Plastic Reconstructive & Aesthetic Surgeons meeting, Delhi, Nov 2009 - Prospective dynamic myosonographic abdominal wall study to compare the donor site morbidity after ms-2 TRAM flap and DIEP flap
K Seidenstücker, B Munder, P Richrath, U Legler, A L Mahajan, C Andree
European Association of Plastic Surgeons meeting, Manchester, UK, May 2010 - Improving outcome in SGAP flap breast reconstruction
A L Mahajan, R Sinna, B Vermeulen, K Van Landuyt
British Asscn. of Plastic Aesthetic & Reconstructive Surgeons Meeting,, Sheffield, July 2010 - Are Pfannenstiel scars a boon or a curse for DIEP flap breast reconstructions?
A L Mahajan, A Zeltzer, K E Y Claes, K Van Landuyt, M Hamdi
World Congress on Controversies in Plastic Surgery & Dermatology (CoPLASDy) Barcelona, November 2010 - Aesthetic benefits of lipofilling in secondary shaping of microsurgical breast reconstructions
K Seidenstuecker, M Hagouan, A L Mahajan, T Koeppe, B Munder, CAndree
World Congress on Controversies in Plastic Surgery & Dermatology (CoPLASDy)
Barcelona, November 2010 (Poster presentation) - Complications in free autologous breast reconstruction – how often is surgical intervention warranted and to what degree?
K Seidenstücker, B Munder, A L Mahajan, C Andree
IInd Italian Meeting on Perforator Flaps and Aesthetic Refinements, Bologna, Italy. “Best Paper Prize” November 2010
- Complications in free autologous breast reconstruction – how often is surgical intervention warranted and to what degree?
K Seidenstücker, B Munder, A L Mahajan, C Andree
International Plastic Reconstructive & Aesthetic Surgeons meeting, Vancouver, May 2011 - Microvascular architecture of a DIEP flap harvested from an abdomen with a Pfannenstiel scar.
A L Mahajan, A Zeltzer, K E Y Claes, K Van Landuyt, M Hamdi
European Association of Plastic Surgeons meeting, Mykonos, Greece, June 2011. - Abdominal seroma formation following DIEP flap harvest – analysis of influencing factors and development of a predictive formula
K Seidenstücker, B Munder, A L Mahajan, C Andree
European Association of Plastic Surgeons meeting,, Munich, Germany May, 2012 - The SGAP flap
A L Mahajan
French Perforator Flap (ACRWP) course, Amiens, France, June 2012 - Technical refinements of Reduction Mamaplasty
A L Mahajan
BODY 2012 meeting, London, November 2012 - Autologous pectoral fascia in implant-based breast reconstruction.
O’Neill TB, Mahajan A L
IAPS Meeting, Galway, Ireland, May 2013 - Technical Refinements of Reduction Mammaplasty.
Scheven D, O’Neill TB, Holmes W, Akhtar A, Mahajan A L
IAPS Meeting, Galway, Ireland, May 2013 - Aesthetic Surgery – Dawn to a new you
A L Mahajan
ATMG Meeting, Alton Towers, UK September 2013 - Breast reduction innovations
A L Mahajan
Byron Bay Meeting, Australia, March 2015 - The Pectoral fascia flap in breast reconstruction
A L Mahajan
Byron Bay Meeting, Australia, March 2015 - The adjustable breast reduction marker
Ajay L Mahajan
BAPRAS meeting, Birmingham, November 2015